GRAND JUNCTION, Colo. (KDVR) — A Mesa County Sheriff’s deputy who nearly died from COVID-19 in 2021 is suing the third-party benefits administrator that denied his workers’ compensation claim last year.
“Sometimes, I feel like it would’ve been better off if I had just died,” said Travis Crawford, 34, who said he believes he contracted the illness while working in the jail.
According to the lawsuit, Crawford alleged that Tristar Risk Management, a workers’ compensation insurance company, “unreasonably denied (Crawford’s) workers’ compensation claim” and violated a law that prohibits insurers from “denying claims without conducting a reasonable investigation based on all available information within the timeframes required by the Workers’ Compensation Act.”
Tristar Risk Management declined to discuss the case, citing privacy issues.
“In addition to privacy laws, it is Tristar’s corporate policy not to make public comments regarding confidential information as to whether any person has filed a claim, whether a claim is pending, or the status of any such claim,” Don Nungesser, associate general counsel for Tristar Insurance Group, wrote in an email.
The Mesa County Sheriff’s Office also declined an interview with the Problem Solvers.
“Mesa County is not able to comment regarding issues that are the subject of active or potential litigation,” said John R. Rhoads, the assistant county attorney.
‘I didn’t have the energy to roll over’
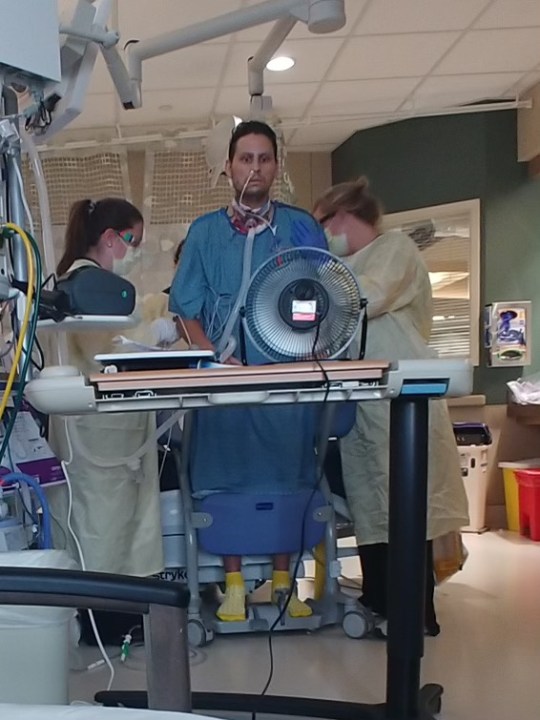
Crawford, who had worked as a county jail deputy since 2017, became sick with COVID-19 in June 2021.
His illness was so severe that he spent nearly three months in the hospital. Crawford was not vaccinated at the time he got sick.
“I just had no energy left in my system, and it felt like my body wouldn’t function,” he said. “They told me to roll over. I didn’t have the energy to roll over.”
At times, he contemplated suicide. He compared himself to a trapped coyote that gnaws off its own leg. “I was that animal, trying to escape at any cost. The pain was horrendous,” he said.
The Mesa County Sheriff’s Office terminated Crawford’s employment during his recovery because Crawford was never well enough to return to work.
“I certainly could not have fought with an inmate. I certainly could not have wrestled with somebody or gained arrest control or done a defensive tactics takedown on someone. Not now,” he said. “They let me keep my badge. They told me that I was a member of their family. They said that they weren’t doing this willingly, that they had to let me go because of my medical conditions,” Crawford said.
Medical treatment limited on Medicaid
Crawford told the Problem Solvers he used all of his family medical leave and some bonus time the sheriff’s office approved while he was fighting for his life.
“I’m depressed, and I’m going through therapy, trying to manage and mitigate all that, but I have to pay for therapy out of pocket. I have to do all this stuff on my own,” he said.
Crawford said doctors also suggested a lung transplant — although he decided against it — after he spent time on a ventilator and received ECMO therapy, a life-support procedure that utilizes a heart and lung bypass machine while those organs are too weak.
“(The benefits administrators) are sitting there making it so that I don’t get benefits when everyone that works there (at the jail) knows that I got (COVID-19) There,” Crawford said.
Crawford said he is currently on Medicaid and receiving a long-term disability benefit, which is different from the continuing care provided by workers’ compensation.
“I wouldn’t have had to go on to Medicaid. And there’s specialists that I haven’t been able to see because I’m on Medicaid,” Crawford said.
He said his physical therapy visits are limited because of his current coverage.
“I went through this awful, traumatic experience. I still need physical therapy, but I’m going to run out of visits, and workers’ comp would be responsible for covering that,” he said. “They’re also responsible for paying out the amount that I became disabled.”
‘I was still dying in the hospital when these outbreaks were happening’
Crawford claimed he became ill with COVID-19 because he worked at the jail.
Because he also attended his grandfather’s funeral in the days prior to his diagnosis, Crawford must prove he didn’t get COVID-19 at a family gathering.
According to the lawsuit, Crawford said his diagnosis came after “working directly with inmates and other staff members that had contracted COVID-19, consisting of 22 active COVID-positive inmates, six COVID-positive staff members and 13 symptomatic inmates.”
The state health department also documented an outbreak at the Mesa County Sheriff’s Office on June 9, 2021.
In his workers’ compensation filings, Crawford reported working in the jail on June 14-15, 2021, attending a dinner on June 18, 2021, and developing COVID-19 symptoms on June 19, 2021.
He also reported that he “traveled for a funeral for his grandfather on June 11-13. There were approximately 30 people at the gathering. No other persons present at that funeral were ill or later became ill with COVID-19 other than (Crawford), and later his father and son.”
Undersheriff suggests Crawford’s illness happened ‘in the line of duty’
In a March letter to the federal Bureau of Justice Assistance Public Safety Officers’ Benefit Program, Undersheriff Matt King wrote that Crawford’s illness “fits all the criteria to be considered a disability that occurred in the line of duty per BJA’s guidelines.”
According to King’s letter, to qualify for PSOB benefits, “a disability from COVID-19 is presumed to have occurred in the line of duty if two conditions are met: (1) the officer engaged in line of duty actions between January 1, 2020, and December 31, 2023, and (2) the officer was diagnosed with COVID-19 during the 45-day period following the law (sic) day of the officer’s duty.”
The lawsuit references the undersheriff’s findings and says the third-party workers’ compensation benefits administrator should have considered the undersheriff’s findings rather than continuing to deny Crawford’s claims.
“Mesa County affirmed (Crawford’s) COVID was work-related on March 4, 2022,” the complaint says. “The purpose of the Workers’ Compensation Act is to help injured workers by promptly providing them with all the benefits available under the act, without the need for any litigation. Tristar and Mesa County are presumed to know what is in their own files, and each other’s files,” it continued.
“Defendant Tristar, despite knowing that Plaintiff’s COVID was caused by his employment, continued to deny Plaintiff’s claim for workers’ compensation benefits,” the suit alleges.
“I was still dying in the hospital when these outbreaks were happening, and they’re going to sit there and try to argue that this wasn’t a line of duty accident?” Crawford said.
Crawford also said he believes that chemical munitions training approximately two weeks before his diagnosis weakened his lungs, making them more susceptible to the sickness.
“I was exposed to CS tear gas and OC vapor,” Crawford said. “I took a deep breath on both exposures, and as a result, I had a cough from that point all the way to my diagnosis of COVID,” he said.
“There is no doubt in my mind that he caught this at the jail,” said Megan Robinson, Crawford’s girlfriend. “For them to think that he caught this in the community is them thinking that the jail is a cleaner environment than the community, a place where they throw feces.”
Nearly 72% of COVID workers’ compensation claims denied
Workers’ compensation exists to compensate people for medical costs and lost wages when they’re injured on the job, according to Paul Tauriello, the director of Colorado’s Division of Workers’ Compensation.
“The problem is that the burden is always on the injured worker to show that the disease or the injury occurred during the course or scope of their employment,” Tauriello said. “Falling off a scaffold? That’s fairly easy to show.”
Tauriello said proving one acquired an illness at the workplace is much harder.
“Early in the pandemic, it was a lot easier because it was not what we call a community spread,” he said.
Between March 9, 2020, and April 30, 2022, insurers have denied 8,662 of the 12,035 COVID-related workers’ compensation claims filed in the state, including 39 claims for people who died.
The statistics do not include federal employees who filed claims.
“The denial rate has actually gone up over time,” Tauriello said, “and we believe that this is a direct correlation with the fact that the disease has spread that much further in the community, outside of people’s workplaces, therefore making it that much harder to prove that it was a work-related exposure,” he said.
What can you do when workers’ comp is denied?
The first step an employee can take after a denial includes pursuing a hearing in front of a judge who will weigh the evidence, Tauriello said.
Where one works — like a jail or healthcare facility — would be a legitimate basis to determine whether it was more likely than not to have been the factor that contributed to a person becoming sick, he said.
“Both sides would be expected to put up evidence to show their particular case, to make their case,” he said. “We’ve seen things where insurance companies have gone to such lengths as asking for people’s phone records to see where they have traveled in the past week or so, and if they see that they have been to a concert, for instance, or where there’s been a large gathering of people, they may decide to present that as evidence to show to a fact-finder, a judge, ‘Look, there was other exposures here,'” he said.
A judge will make a determination based on the evidence, but that determination can later be appealed.
“It is appealed on the record, meaning no new evidence is added on appeal,” Tauriello said.
He said the information that was already reviewed by the initial judge would then be reviewed on the basis of conclusions of law.
A person going through an appeal process should be prepared for a matter of months, at least, Tauriello said. He said the process could exceed a year or more.
“At any point, the parties can reach an agreement,” he said.
He said anyone who has questions about how the system works and the status of their claim can confirm that through the Colorado Workers’ Compensation Division at 303-318-8700.